The Dementia Fall Risk Statements
The Dementia Fall Risk Statements
Blog Article
What Does Dementia Fall Risk Do?
Table of ContentsGetting My Dementia Fall Risk To WorkAbout Dementia Fall RiskThe Best Strategy To Use For Dementia Fall RiskNot known Incorrect Statements About Dementia Fall Risk
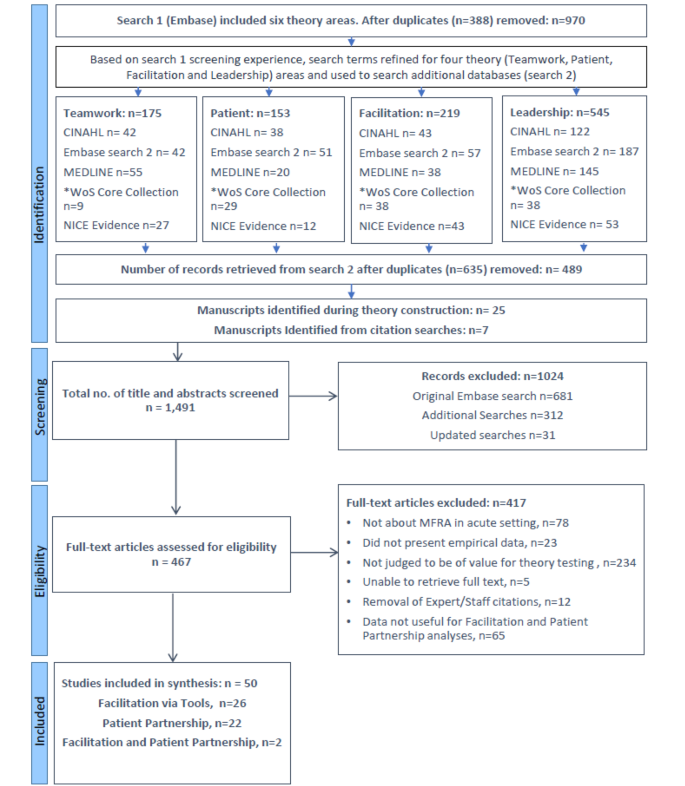
A loss risk analysis checks to see exactly how likely it is that you will certainly drop. The assessment generally consists of: This consists of a series of questions regarding your general wellness and if you have actually had previous falls or troubles with balance, standing, and/or walking.STEADI includes testing, examining, and intervention. Treatments are suggestions that might decrease your danger of dropping. STEADI consists of three actions: you for your danger of succumbing to your danger variables that can be enhanced to attempt to avoid falls (for instance, balance troubles, damaged vision) to minimize your threat of falling by utilizing reliable methods (for instance, giving education and sources), you may be asked numerous questions including: Have you dropped in the previous year? Do you feel unstable when standing or walking? Are you fretted about falling?, your copyright will check your stamina, balance, and stride, utilizing the following loss evaluation tools: This examination checks your gait.
After that you'll take a seat once again. Your provider will certainly inspect for how long it takes you to do this. If it takes you 12 secs or more, it might suggest you go to greater danger for an autumn. This examination checks toughness and balance. You'll rest in a chair with your arms went across over your chest.
The placements will certainly obtain more difficult as you go. Stand with your feet side-by-side. Relocate one foot midway onward, so the instep is touching the big toe of your various other foot. Relocate one foot completely before the other, so the toes are touching the heel of your various other foot.
What Does Dementia Fall Risk Do?
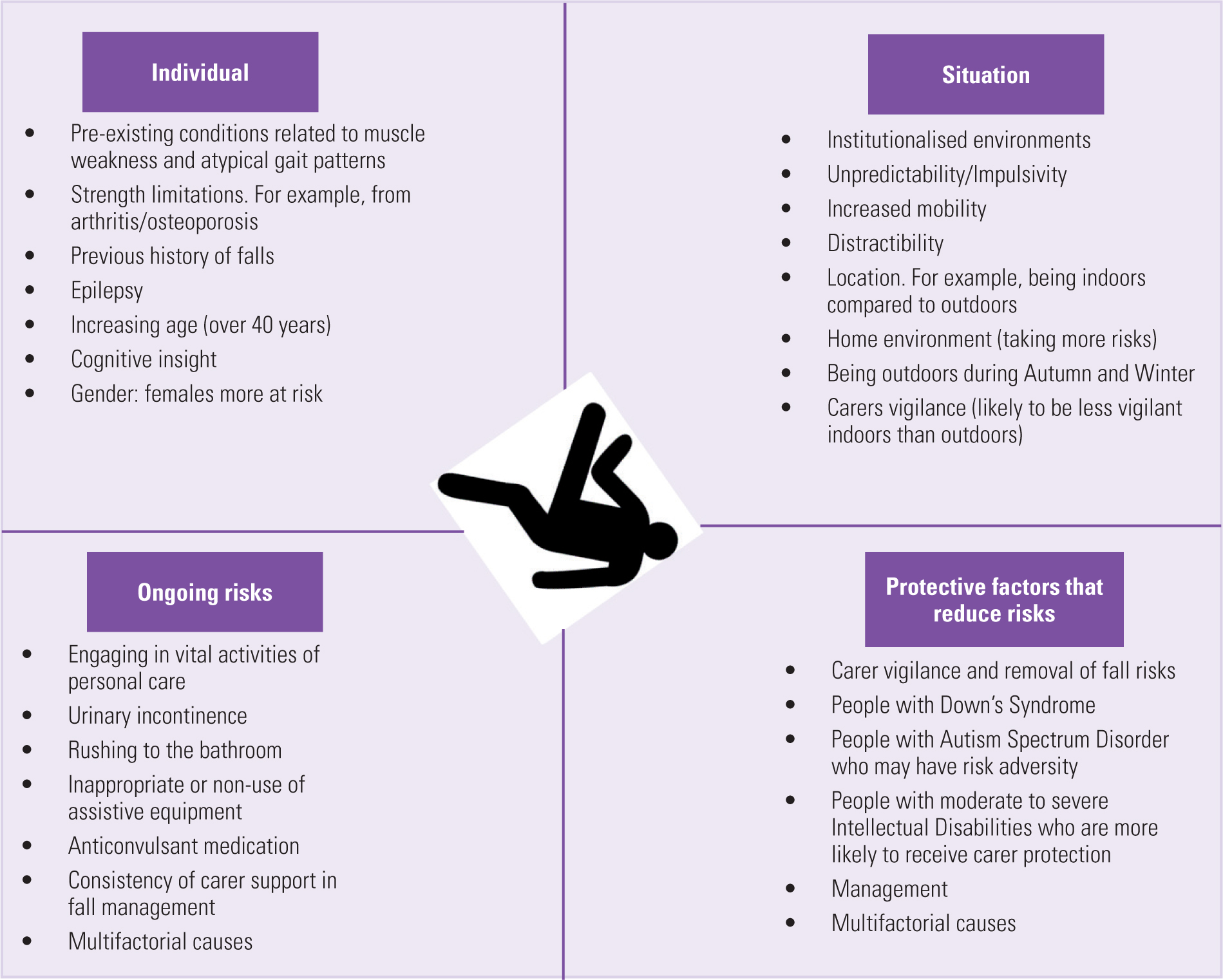
Most falls take place as a result of several adding variables; as a result, managing the danger of dropping begins with recognizing the variables that add to drop danger - Dementia Fall Risk. Some of one of the most appropriate danger elements consist of: Background of previous fallsChronic clinical conditionsAcute illnessImpaired stride and equilibrium, reduced extremity weaknessCognitive impairmentChanges in visionCertain risky drugs and polypharmacyEnvironmental elements can additionally increase the risk for falls, consisting of: Inadequate lightingUneven or harmed flooringWet or unsafe floorsMissing or harmed handrails and get hold of barsDamaged or poorly fitted tools, such as beds, wheelchairs, or walkersImproper use assistive devicesInadequate supervision of individuals living in the NF, consisting of those who exhibit hostile behaviorsA successful autumn danger management program requires an extensive medical evaluation, with input from all participants of the interdisciplinary team
The care strategy need to also include interventions that are system-based, such as those that advertise a secure atmosphere (appropriate lights, hand rails, get hold of bars, etc). The effectiveness of the treatments should be assessed occasionally, and the care plan changed as needed to reflect changes in the autumn risk assessment. Executing an autumn threat monitoring system utilizing evidence-based best method can lower the occurrence of drops in the NF, while limiting the capacity for fall-related injuries.
A Biased View of Dementia Fall Risk
The AGS/BGS standard advises evaluating all grownups aged 65 years and older for loss danger every year. This screening contains asking clients whether they have fallen 2 or more times in the past year or sought clinical interest for click site an autumn, or, if they have actually not fallen, whether they really feel unsteady when strolling.
People who have actually fallen visite site as soon as without injury should have their balance and gait examined; those with gait or balance problems need to receive extra evaluation. A history of 1 autumn without injury and without gait or balance troubles does not require further assessment past ongoing annual loss risk screening. Dementia Fall Risk. An autumn risk analysis is required as component of the Welcome to Medicare exam
The Only Guide to Dementia Fall Risk
Documenting a falls background is one of the top quality indications for autumn prevention and monitoring. copyright drugs in specific are independent predictors of drops.
Postural hypotension can typically be reduced by reducing the dose of blood pressurelowering drugs and/or stopping medicines that have orthostatic hypotension as a side impact. Usage of above-the-knee assistance hose pipe and resting with the head of the bed raised may likewise decrease postural reductions in high blood pressure. The suggested aspects of a fall-focused checkup are revealed in Box 1.

A yank time more than or equivalent to 12 secs suggests high fall risk. The 30-Second Chair Stand examination analyzes lower extremity strength and equilibrium. Being not able to stand up from a chair of knee elevation without making use of one's arms suggests raised loss danger. The 4-Stage Balance test analyzes static balance by having the person stand in 4 placements, each progressively a lot more tough.
Report this page